Dr. Manel Escobar has contributed a new case: 23-year-old woman with cough and low-grade fever.
1. Tuberculosis
2. Sarcoid
3. Lymphoma
4. None of the above
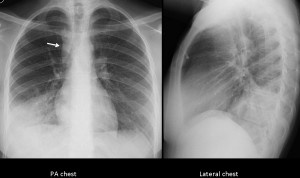
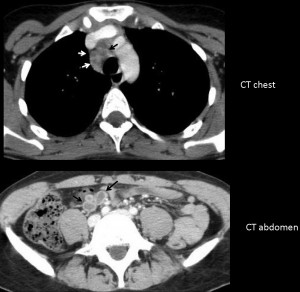
PA chest shows air-space disease in the right lower lobe, with widening of the para-spinal line (arrow) suggestive of mediastinal lymphadenopathy. Axial CT confirms enlarged paratracheal lymph nodes with hypodense centre (arrows), also visible in the abdomen (arrows).
These findings should suggest tuberculosis as the first possibility. Although TB usually affects upper lobes, involvement of lower lobes should not exclude it.
Final diagnosis: active TB. Congratulations to all of you who made the diagnosis. Muppet believes this was an easy case, considering that most of you made the right diagnosis. The next case will be more difficult because it commemorates Muppet’s 25th anniversary.
Teaching point: lymph nodes with hypodense centre may occur in several processes (treated tumours, Whipple’s, etc.), but in the appropriate clinical situation, the first diagnostic consideration should always be tuberculosis.
Parenchymal consolidation of the basal segments of the right lower lobe with right-sided mediastinal lymphadenopathy. The nodes have a hypodense center (necrosis).
I choose No. 1 – (primary) tuberculosis.
Paratracheal adenopathy (with aparent necrotic center on CT).
Right lower lobe consolidation with air bronchogram.
I wouldn’t expect necrotic adenopathy in Sarcoidosis; the consolidation with alveolar characteristic is not frequent as far as Im concerned (would be alveolar Sarcoidosis); and moreover use to be bilateral and with upper lobes predominance.
I also wouldn’t expect necrotic adenopathy in Lymphoma (and I would prefer more extensive adenophatic consolidation). The primary lung lymphoma can appear as an air space consolidation with bronchogram (usually multiple I think). With this also wouldn’t consider lymphoma in my initial diagnosis.
Tuberculosis…could be, but I would prefer the consolidation in an upper lobe.
Summarising, I don’t like the three first options Muppet gave us and I will choose 4 thinking then in an ATYPICAL NON TUBERCULOUS MYCOBACTERIAL INFECTION.
Can you discriminate between typical and atypical TB by looking at the radiographs?
Not really, it only was an hypothesis. If it is TBC its quite clear that its a primary infection. The most frequent location is upper lobe or superior segment of the inferior lobe. Other mycobacteria also are more frequent in the upper lobe, but as far as Im concerned its not as constant finding as in TBC. That s why I chose Atypical mycobacteria not TBC.
Anyway, the answer is no, I cant discriminate, only “play” with tendencies and frequencies of each pathology.
And here the topic that it is more frequent and atypical manifestation of a typical pathology than typical manifestation of atypical pathology goes against me, I know, but Muppet cases are so tricky… That I had to do something… Hehe
Partiamo dal dato clinico : il soggetto è giovane e la febbre lieve( nonostante l’estesa area di consolidamento parenchimale,postero-basale dx).Lo svasamento mediastinico è omolaterale, di natura linfo-adenopatica e con caratteristiche di necrosi-colliquazione centrale, senza tendenza alla confluenza. C’è un ultimo dato, forse “la chiave” di lettura: il catetere venoso in LL( da nutrizione venosa centrale?). Allora io penso ad un complesso primario TBC in soggetto immuno-depresso.
mainly i think of TB if its of east parents or recently visist
but lymphoma more because of low grade fever
Yes, patient was from the East
TB
widening of right paratracheal stripe due to lymphadenopahty with consolidation in basal segments of right lower lobe. The enlarged nodes shows central hypodense area.
Prominent horizontal fissure.
TB is the most probable diagnosis.
Pneumonic process in the RIL (mostly lateral and posterior basal segment). Confluent adenopathy in right paratracheal region, with necrosis / caseification. Lymphoma usually does not have necrosis unless treated. My impression is primary pulmonary tuberculosis – although at quite a advanced age for my country ( 🙂 )
Tuberculosis-necrotic lymph nodes in mediastinum is the clue
Sarcoid
Enhanced CT is routine in most places when studying the mediastinum. I prefer to decide depending upon the findings in the chest radiographs.
I don´t believe HRCT will be useful in this case. Regular CT is good enough to demonstrate the infiltrate in the RLL and to rule out any endobronchial lesion
Opps! wrong answer
Don’t you think hypodensity of lymph nodes goes against sarcoidosis?
I agree with all of the above have already written, another option although it does not fit necrotic lymph node.
Saccular or cystic bronchiectasis….
It seems to me that there is dilatation of the bronchi in the middle lung field + cough
Consolidation of the right lower field (pneumonia) plus enlarged right paratracheal stripe (CT shows linfoadenopathy with ipodense core). No other signs of pathology seem to be present at plain films.
Quite difficult radiologic diagnosis, I agree with others friends, TB is the most probable diagnosis.
I don’t understand why did you performed a contrast enhanced CT, maybe because of the widening of the right paratracheal? Could be useful an HRCT?
Thank you Dr Caceres
Enhanced CT is routine in most places when studying the mediastinum. I prefer to decide using IV contrst depending upon the findings in the chest radiographs.
I don´t believe HRCT will be useful in this case. Regular CT is good enough to demonstrate the infiltrate in the RLL and to rule out any endobronchial lesion
There are mediastinal and hilar lymphadenopathy, alveolar pattern and pleural efusion. They are consistent with TB or Lymphoma.
Hypodense lymph nodes can be seen on TB. It could be thought about seminoma if she was a male. But…she isn´t it as I am. As far as I know germinal ovariam tumours doesn´t cause hypodense lymph nodes.
TB seems the best posibility. I would try to exclude AIDS.
D’accordo sul complesso primarioTBC: ma quello che non è stato spiegato è perchè un complesso primario deve ” presentarsi” con un focolaio di addensamento bronco-pneumonico: a meno che non ci sia una concomitante immuno-deficienza, primitiva o sec ondaria! Quale è inoltre il ” significato” del catetere venoso che si vede in LL ed alla TC? Vogliono gli illustri colleghi darne una possibile spiegazione?.Grazie: Attendo la prossima sfida!!! Forza ITALIA!!!!
I enjoyed the blog and content. From now on I will frequent the blog and I will comment discussing the post. I do not write well in English, but this will help me to keep learning.