Dear Friends,
Muppet is very happy to have reached the 25th case and hopes for twenty-five more!
Forty-nine-year-old woman with persistent cough for the last two months.
Diagnosis:
1. Carcinoma
2. Tuberculosis
3. Bronchiectasis
4. None of the above
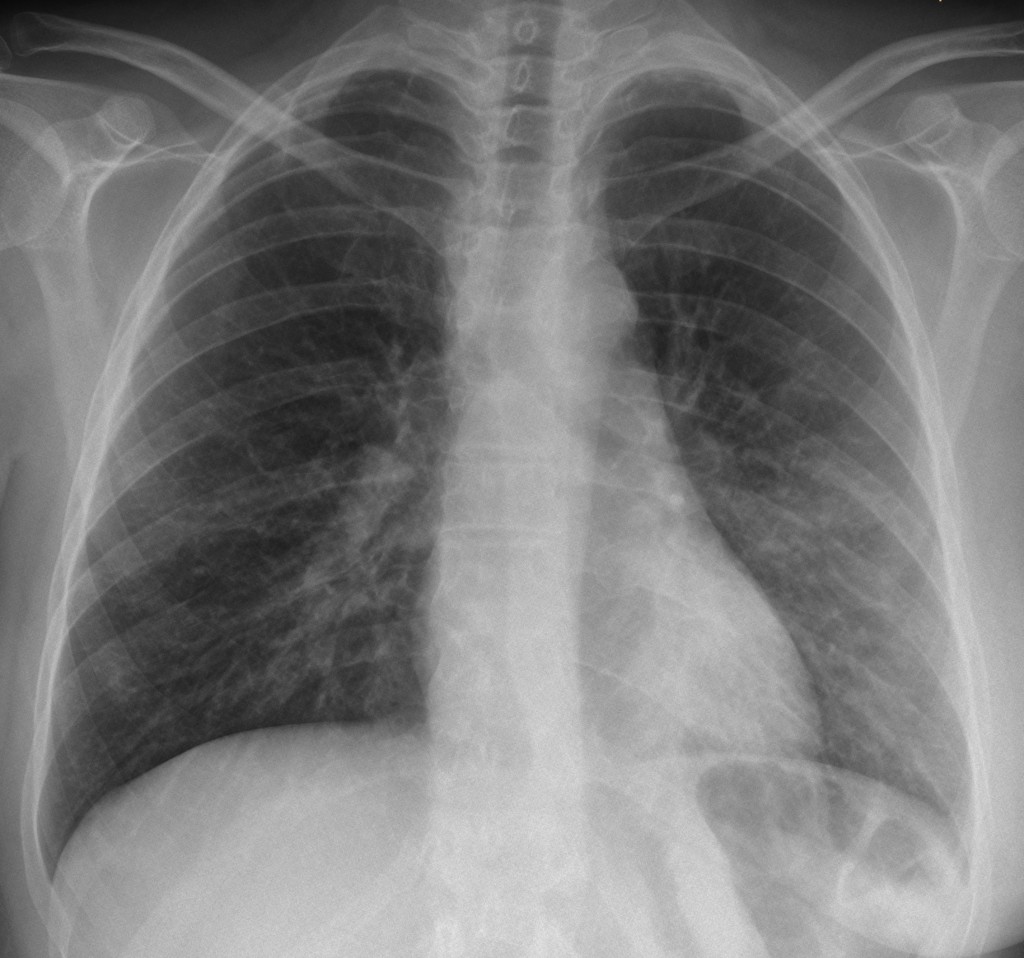
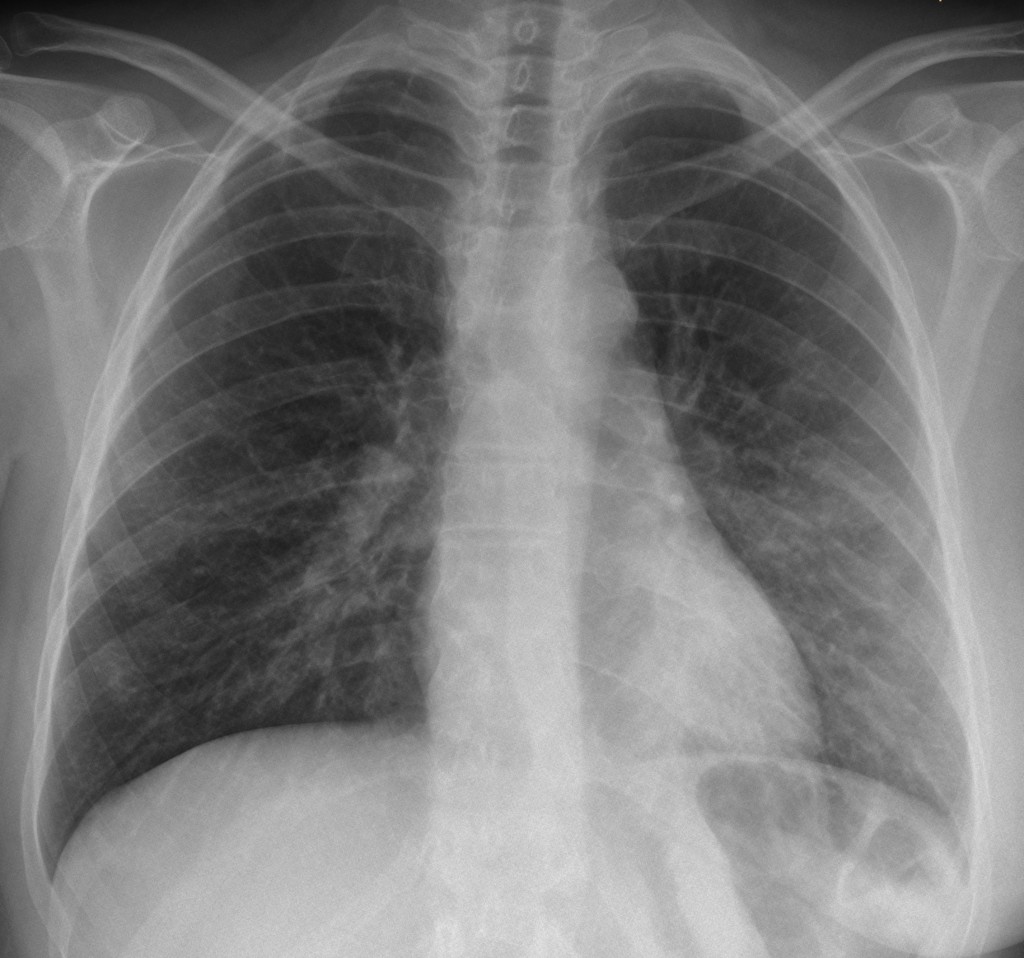
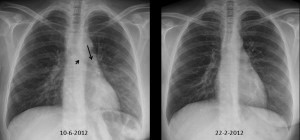
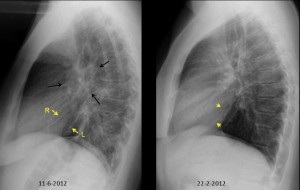
49-year-old woman, PA chest
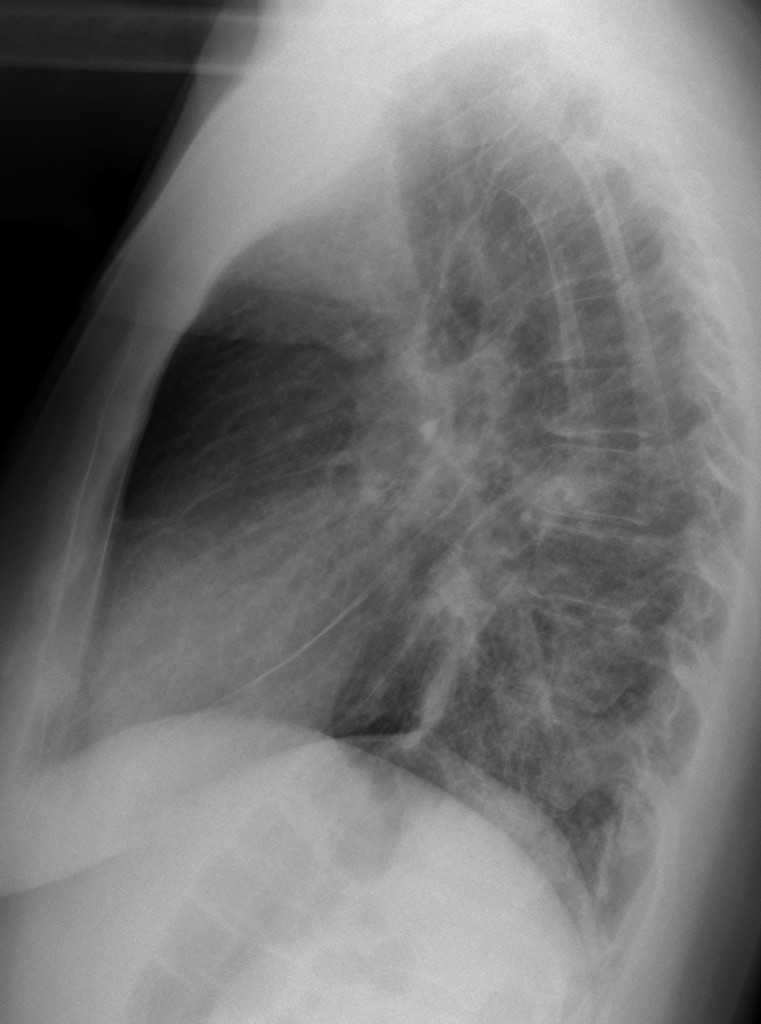
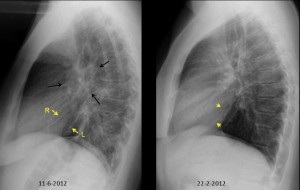
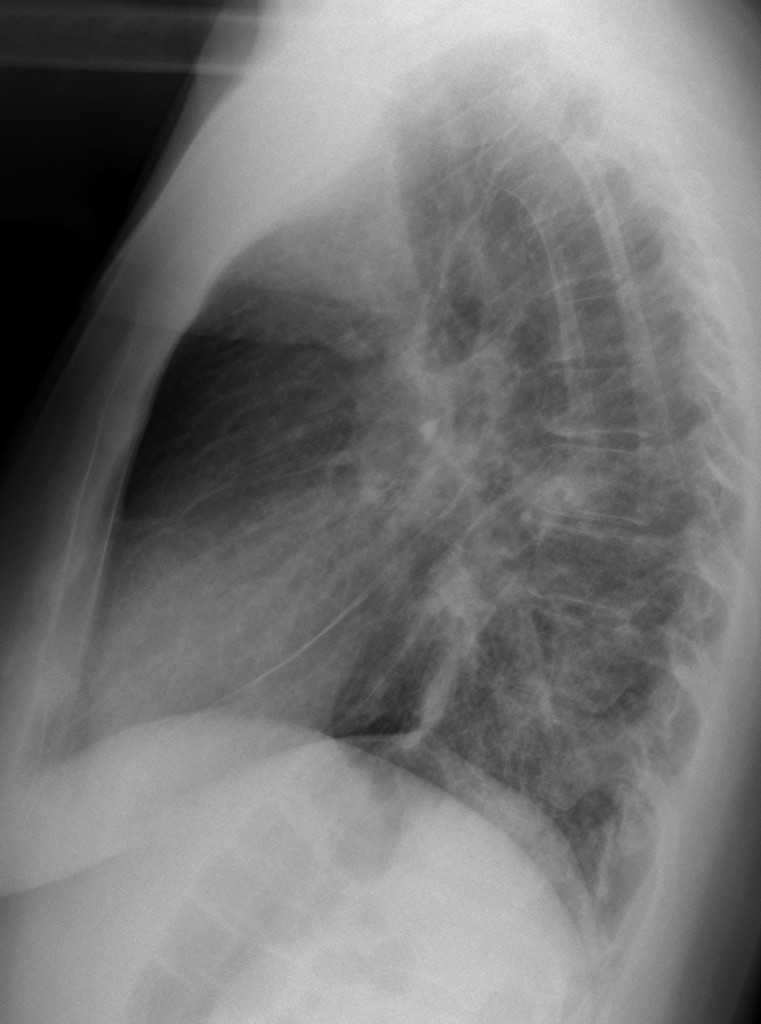
49-year-old woman, lateral chest
Click here for the answer to case #25
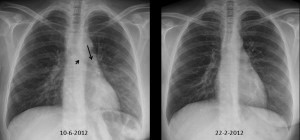
PA chest shows non-descript opacity in LLL with moderate downward shift of the left hilum (arrow), partially hidden behind the heart shadow, accompanied by a vertically oriented left main bronchi (arrow). The lateral film shows a hilar donut sign (arrows) and posterior displacement of the left major fissure (yellow arrows). These signs indicate moderate volume loss of LLL and they are evident when compared with radiographs taken four months earlier.
In a patient with mastectomy (absent right breast in PA film), the most likely diagnosis is either metastatic disease or primary bronchial tumour.
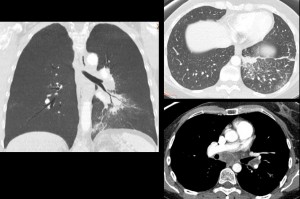
CT shows peribronchial metastatic infiltration of LLL bronchus with lymphangitis and mediastinal and hilar lymph nodes with hypodense centre, probably due to chemotherapy. Previous CT was normal.
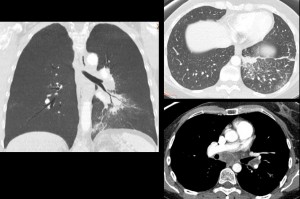
Final diagnosis: metastatic carcinoma of the breast.
Teaching point: this case illustrates the main findings of LLL collapse. Conventional radiography offers a lot of information if we look for it (see Marius’ interpretation above).


Non TBC:anomala come presentazione e senza adenopatia. Non Cr , tipo bronchiolo-alveoare, senza altri dati clinici( es: perdita di peso, febbricola…). Non bronciectasie, perchè mancano gli altri segni della BCO. Difficile allora la valutazione sulla base della semplice Rx: aspetto a ” ground-glas” postero-basale sx. I risultati della BAL ed i test di funzionalità respiratoria( di tipo ad es. restrittivo)? Forse una pneumopatia di tipo interstiziale(IIP).
It seems that there are bibasal (with left predominance) opacities consisting of some irregular alveolar consolidation (Left), some small lines and nodules and areas of ground glass. It suggest to me a kind of inflammatory- infectious process bronchiolitis like probably with some small infected bronchiectasies.
And then a little bit imaginitve signs, but I don’t clearly see the gastric air camera and -maybe imaging again- some “strange” air in retrotracheal and retrocardiac and right hila and cardophrenic sinus. No clear air fluid levels in mediastinum.
Can I ask if she suffers any swallowing disorder?
No swallowing disorder.
malignancy.
reasons:
1. Right breast shadow is not seen by my eyes.
2. Reticular shadows in both lower zones – ?BAC or secondary to film rotation. The lateral view seems to say that the shadows are not due to rotation.
3. Left upper zone- Is there an apical capping or bony involvement?
Malignancy relapse in a previously operated Ca breast?
Alveolar infiltrate in the inferior left lobe that suggests pneumonia.
considering that the condition lasts 2 months is more probably to be a subacute alveolar process for example bronchoalveolar carcinoma?.
Dr. House has a reputation and should give a reasoned explanation of his diagnosis
I agree, the right breast is missing. Metastatic disese is a possibility.
Left hilum is slightly displaced and lower…
I choose no. 1: carcinoma.
Do I see Kerley lines ?
Both mayor fissures thickened.
Bulge at the aortopulmonary window (adenopathy)
Smells to lynphangitis carcinomatosis.
Congratulations to muppet !
We believe it could be a malignancy relapse of previously operated breast carcinoma.
There are bronchi inspissated with mucus in both mid and lower lung zones. The bronchi do not taper peripherally. The lung apices are spared. I’ll go with option 3 : bronchiectasis.
Donut sign +close to 90 degrees angle of carina + bulging aorto-pulmonary window sugest ADP. There is a segmental atelectasis in the anterior basal segment of the LIL creating a diaphragmatic peak on profile, seems to be in relation with a central irregular opacity of about 2 cm (central carcinoma?). There’s also a 1 cm pulmonary opacity projected over the anterior arch of the 4th left rib that also seems to belong to the LIL. Septal thickenings at both pulmonary apices. Reticular interstitial pattern on all of the LIL – lymphangitis? Needs chest CT with contrast.
Be patient. CT will be shown shortly
There is lost of volume at LLL and right mastectomy. I’d think about endobronchial metástases. There also are modules at LLL . They could be lung metastases of localized linfangitis
get cheap burberry outlet online at my estore hSXZozKR http://www.burberryoutlet-online.net/
you must read where to buy louis vuitton online for gift