ECR 2013 Focus: Organs From A to Z: Heart
Heart disease affects a very large number of people worldwide, and the consequences can be serious and even lethal. Here, and perhaps more than in many other areas of medicine, imaging has helped to improve treatment and prevention. It does so by detecting the disease at an early stage, sometimes even before its emergence, especially in patients at risk of ischaemic heart disease.
Today, diagnosing cardiac patients has become routine for many radiologists. However, some of them may not know of recent developments in this field and they may need to refresh their knowledge. A panel of experts will update both general and specialised radiologists with the latest information available on cardiac imaging, during the dedicated Mini Course ‘Organs from A to Z: Heart’ at ECR 2013. After an introduction to heart anatomy and the main imaging protocols, the course will focus on valvular diseases and cardiomyopathies; two pathologies commonly encountered in radiology practices.
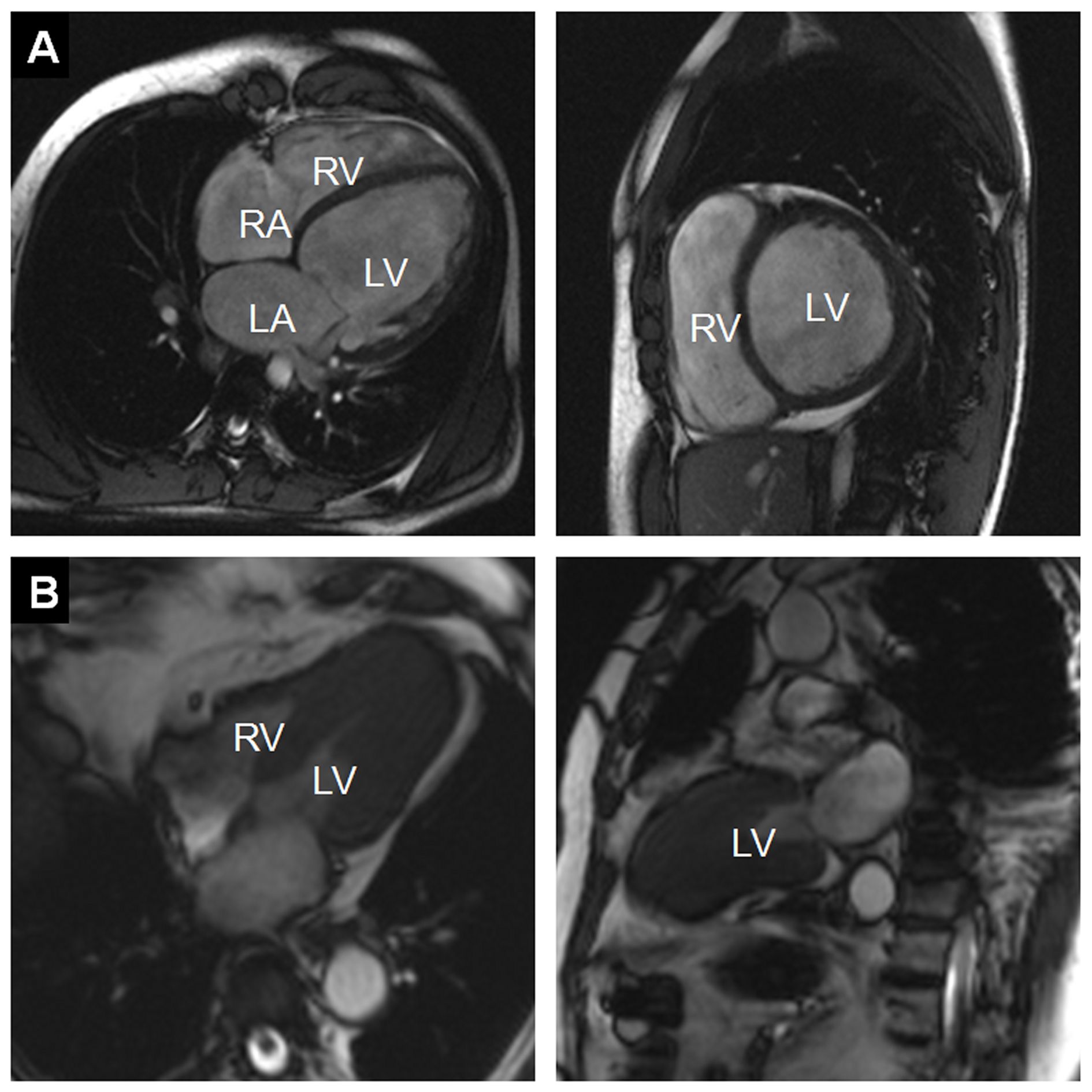
Figure 1:
A) Example of a dilated cardiomyopathy (DCM). Cine-MR images in four-chamber view (left) and short-axis view (right) at end-diastole show significant dilatation of the LV cavity. Ejection fraction was <35% in this patient. (RA = right atrium; LA = left atrium; RV = right ventricle; LV = left ventricle)
B) Example of an asymmetrical, apical hypertrophic cardiomyopathy (HCM). Cine-MR images in a four-chamber (left) and two-chamber view (right) in systole show a markedly thickened left ventricular myocardium predominantly of the apex, as compared with the basal segments (RV = right ventricle; LV = left ventricle).
“Anyone who has MRI equipment and has experience of cardiac cases is likely to be asked by a cardiologist to diagnose one of these patients someday,” said Konstantin Nikolaou, professor of radiology and vice chair of the Department of Clinical Radiology at Munich University Hospital in Germany. MRI allows radiologists to assess cardiomyopathies and valvular disease with a very high level of precision, even though echocardiography – especially in skilled hands – often proves sufficient. “MRI is very good at quantifying the degree of a cardiac valve problem. By using MRI, you can determine the direction and quantity of blood flow, and thereby assess a valvular insufficiency or stenosis with great accuracy,” explained Nikolaou, who will chair the Mini Course at the ECR.
MRI can also be crucial in the diagnosis of congenital heart diseases, in cases where ultrasound proves inconclusive. But the problem with MRI in cardiac imaging remains its availability; often limited to universities or dedicated centres, and often with long waiting lists. Congenital diseases are usually assessed in babies or very young children, for whom it is almost impossible to lie still in an MRI scanner for 45 minutes without sedation or general anaesthesia, which can present a risk for children. Consequently, radiologists may choose to use CT in younger patients, as it offers rapid diagnosis and has become safer in recent years, with a significant improvement in dose reduction strategies.
“We perform more and more CT examinations to assess congenital heart disease in both adults and younger patients, even new-borns, because new acquisition techniques use a lower radiation dose. CT gives you a very fast diagnosis. Sometimes you can’t or don’’t want to sedate a little child for 45 minutes for an MRI scan. The patient may also be too sick to lie still for so long. CT has thus become an alternative, even if MRI remains the first option,” Nikolaou pointed out.
The third part of the session will focus on ischaemic heart disease, the main cause of death in western countries, before cancer. Catheter angiography performed by a cardiologists remains an excellent way to assess the risk of developing a cardiac event, but it is an invasive procedure with risks. Here as well, CT presents a number of advantages. It has been used for over 20 years to provide non-invasive examinations of the coronary arteries. Traditionally, CT’s two main applications in cardiac imaging are calcium screening, which measures the amount of calcium in the arteries, and coronary CT angiography, which can reveal the degree of stenosis of the vessels.
CT angiography actually goes beyond risk assessment, and is typically carried out in a symptomatic patient with suspected coronary artery disease to exclude stenosis, for instance in a patient presenting with chest pain, but not a typical angina. In such cases, the radiologist might be asked to perform a coronary CT angiography, to prove or exclude the existence of stenosis and further characterise potential disease of the coronary arteries. In addition, researchers have started to use CT to differentiate between types of coronary plaques. Plaques in the vessel wall not only consist of calcium, but also other tissues such as fibrotic, fibro-fatty and necrotic core tissues, all of which may have a predictive value for the patient. “Today, we would hardly make a clinical decision based on CT plaque imaging alone, but it is one of the important topics in cardiac CT research,” Nikolaou said.
Current scientific studies have also been focusing on a more detailed analysis of the myocardium, i.e. applying CT techniques instead of MRI to the depiction of myocardial perfusion defects, in order to gain time in the diagnostic process. “Patients are sometimes referred to nuclear medicine, or for an MRI scan for perfusion tests, when CT angiography results are inconclusive. We now try to get information on perfusion during the CT examination, by adding a CT perfusion scan to angiography,” he said. “This would potentially enable us to get the whole picture in one examination and make a better clinical decision, based on the functional relevance of a given stenosis. Whether these rather new CT techniques will be used in everyday clinical routine is still not clear,” he added. Study results indicate that researchers will probably soon be able to find the perfusion defect caused by a stenosis with CT, Nikolaou believes. “Depending on correct patient selection in accordance with cardiology, I think that we will, in a few years, start to use CT perfusion or CT dual imaging of the myocardium for the assessment of functional relevance of a coronary artery stenosis detected in CT angiography,” he said.
MRI and nuclear medicine tests still set the standard for the assessment of the myocardium in ischaemic heart disease, as both of these imaging modalities can provide very detailed information on the ischaemic myocardium. For instance, in a patient with suspected ischaemic heart disease, MRI can reveal typical lesions in the myocardium caused by an infarct. MRI is also able to help establish whether a myocardial infarction happened recently or a few years ago. “If you use water-weighted images, the presence of oedema in the myocardium means that this is a recent infarct,” Nikolaou said. MRI is the first modality in more complex or known cases of coronary artery or ischaemic heart disease, for instance if a patient received bypass surgery, suffered known infarcts or underwent coronary interventions (e.g. with stent implantation). “CT is good for assessing ischaemic heart disease at an early stage or for a first diagnosis, but MRI does a better job if it is a more complex case. It gives information on the perfusion defect, old events, if the stent is still patent, etc.”, he concluded.
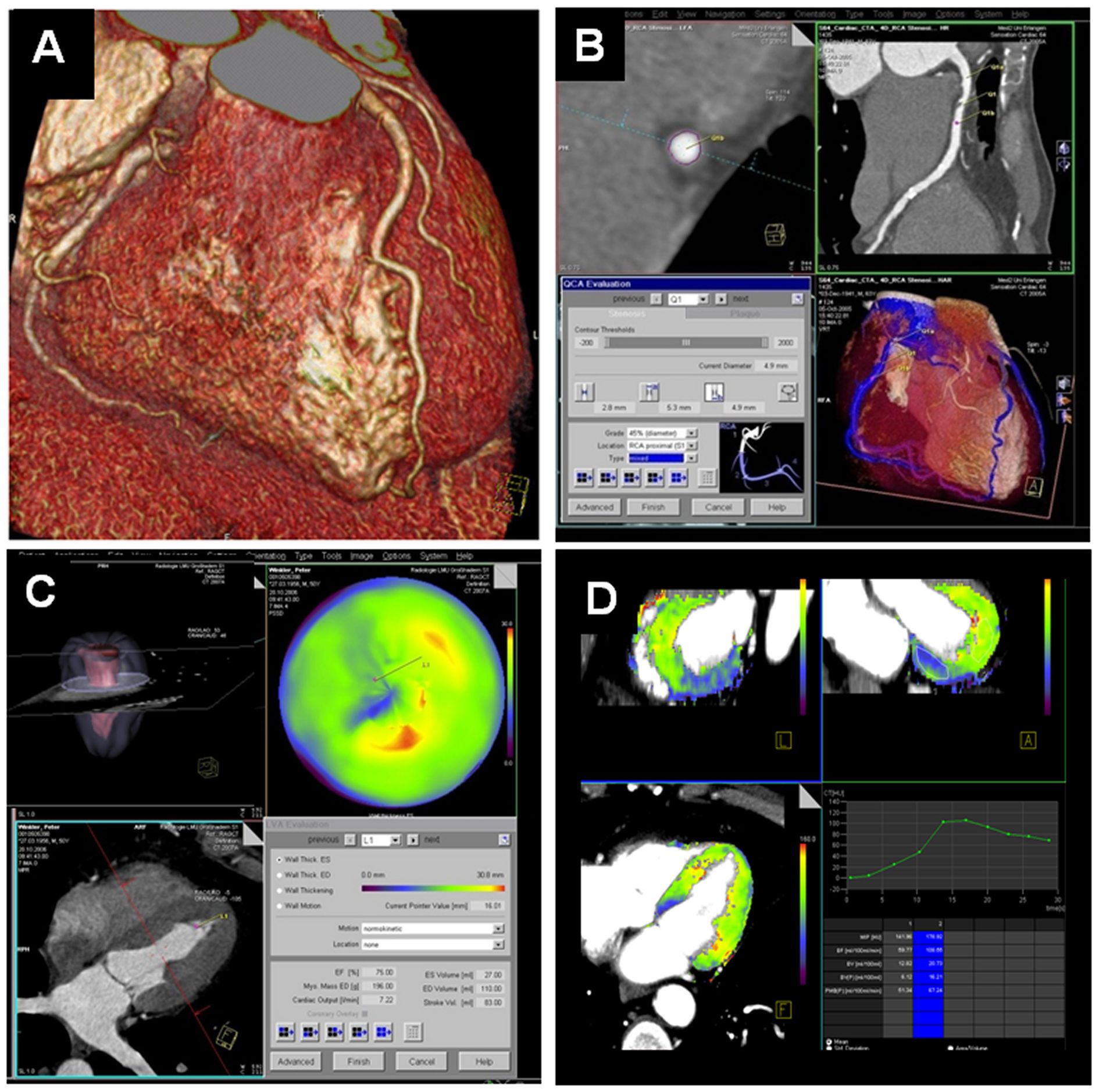
Figure 2:
Today, contrast-enhanced Cardiac CT is mainly used to display cardiac and coronary morphology in non-moving images. Results can be displayed through volume-rendering techniques (A) or dedicated software can be used for a detailed analysis of the coronary arteries and potential coronary artery stenoses, e.g. using curved multiplanar reformats (B). However, Cardiac CT can also analyse cardiac function (global functional parameters as well as regional wall motion, displayed in colour maps, C). Recent developments and research are focusing on the assessment of myocardial perfusion, e.g. using dynamic, time-resolved acquisition modes. This way, blood flow through the myocardium can be displayed in colour maps or in time-density curves, potentially allowing assessment of the haemodynamic significance of a given coronary artery stenosis (D).
Mini Course
Organs from A to Z: Heart
Thursday, March 7, 16:00–17:30
Technical and anatomical fundamentals for imaging the heart
Friday, March 8, 08:30–10:00
Non-ischaemic heart disease
Friday, March 8, 16:00–17:30
Ischaemic heart disease
This article previously appeared in the ECR 2013 Preliminary Programme
All images provided by Professor Konstantin Nikolaou.