Interview: Joanna Fairhurst, consultant paediatric radiologist from Southampton, UK
An interview with Joanna Fairhurst, consultant paediatric radiologist at the children’s radiology department of the University Hospitals of Southampton.
European Society of Radiology: What is paediatric imaging? What age are the patients, and how is it different from regular imaging?
Joanna Fairhurst: Paediatric imaging covers all imaging modalities – plain films, ultrasound, fluoroscopy, computed tomography (CT), nuclear medicine, magnetic resonance (MRI) – undertaken in children ranging from new-born infants to those who are sixteen, or in some centres eighteen, years old. Imaging patients in this age range poses some very specific challenges. First, coming to the hospital can be a very frightening experience for young children, and we need to adapt our techniques to help children feel as secure and comfortable as possible, and we often employ distraction and play therapy to reduce their anxiety and help them cooperate with their examinations. We also try to create a child-friendly environment, by decorating our department and providing toys, but the best way to make our young patients feel at ease is to have radiographers and radiologists who are experienced in, and enjoy working with children.

Joanna Fairhurst is a consultant paediatric radiologist at the children’s radiology department of the University Hospitals of Southampton
The next main difference between paediatric and adult radiology is that we have to be familiar with the imaging appearances of the developing patient – from pre-term infant to adolescent – including many normal developmental variants. We also have to deal with many diseases and pathologies that are specific to children. Unlike other subspecialties within imaging, although some do specialise, most paediatric radiologists are involved with all modalities and all body systems.
Finally, when we image children, we not only have to communicate with young people: very often we also have to interact with their parents and carers, so we must learn to respond to their concerns and needs as well.
ESR: Since when has paediatric imaging been a specialty in its own right?
JF: It could be argued that paediatric radiology is the oldest imaging specialty, dating back to the use of x-rays and the interpretation of the images produced in children’s hospitals in the early 1900s. Many people, however, consider Dr. John Caffey (1985–1978) as the ‘founder’ of paediatric radiology after he published his book Pediatric X-Ray Diagnosis in 1945. Paediatric imaging gained broader recognition in the United States with the founding of the Society for Pediatric Radiology in 1958, and came of age in Europe with the creation of the European Society of Paediatric Radiology in 1963.
ESR: Which imaging modalities are usually used to examine paediatric patients? Does this change depending on the age of the patient?
JF: All forms of imaging are used to examine paediatric patients, but undoubtedly plain radiographs and ultrasound are the current mainstay of imaging in children. There are several reasons for this. Because of their size, children are ideal subjects for the use of ultrasound, and most children can be quickly reassured that this technique is not uncomfortable or painful. The fact that no radiation is involved is also a huge factor in its favour. Although plain radiographs do involve the use of radiation, this is at much lower doses than are required for other forms of imaging, and the diagnostic yield of this form of imaging is particularly high in paediatric practice. Both techniques are readily delivered on the ward, so are ideally suited to imaging very sick neonates and children.
Because MRI requires patients to lie still for many minutes at a time, this imaging modality poses problems for young patients who often find it hard to lie still for even a few seconds. In very young infants we can get around this problem by feeding the patient just before their scan: when securely wrapped in a blanket they often sleep through the examination. However, scanning older infants and young children can require sedation or general anaesthesia, so we try to use other imaging techniques in this age group. Low tissue volumes and relatively small amounts of intra-abdominal fat can also make the interpretation of CT and MRI more challenging in young children, as resolution and soft tissue discrimination are affected.
ESR: Some imaging techniques, like x-ray and CT, use ionising radiation. What risk does this radiation pose to paediatric patients? What kind of safety measures are in place to protect children?
JF: Infants and young children are particularly susceptible to the risks of ionising radiation for a number of reasons. Rapid cell division in the growing child makes them more susceptible to biological effects of radiation, the body’s reparative mechanisms are not fully developed in children, and young people are an order of magnitude more sensitive to radiation than adults. Moreover, a patient exposed to radiation in childhood has a much longer period available for the delayed effects of radiation to be expressed.
Imaging professionals working with children are constantly aware that a major component of their job is to protect their young patients from the risks of radiation exposure. To this end, they ensure that the doses used in imaging techniques that require radiation are kept as low as possible in providing a diagnostic study. This is expressed in the ALARA (As Low As Reasonably Achievable) principle, and is supported by groups such as Image Gently (the Alliance for Radiation Safety in Pediatric Imaging) and EuroSafe Imaging. As well as tailoring exposure factors to patient size, we also limit the area scanned – for example only scanning the level of concern in a trauma patient whose cervical radiographs suggest an abnormality, rather than scanning the whole cervical spine. Most paediatric body CT examinations only require a single-phase post-contrast scan rather than pre-contrast, arterial phase and venous phase imaging employed in adults, which has a dramatic effect on the total radiation exposure.
Reducing the need for repeat exposures due to technical problems can also impact on radiation dose to the patient, and the best way to achieve this is for paediatric imaging to be undertaken by radiographers who are experienced in paediatric practice. Most importantly, however, paediatric imagers ensure that every examination performed on a child using ionising radiation is truly necessary and that the diagnostic information provided by that study will contribute to the management of that patient. Wherever possible, therefore, we will undertake alternative imaging such as ultrasound or MRI.
ESR: Do general radiologists always use lower radiation doses when imaging children; are there any guidelines to follow?
JF: Unfortunately, although all radiologists should adhere to the ALARA principle, not all radiologists are as attuned as they could be to the specific needs of young patients. For example we know that the radiation exposure of children who undergo trauma scans in general hospitals is significantly higher than that experienced by young patients examined in paediatric centres. Many centres that do not routinely image large numbers of children omit to adjust their imaging parameters for the size of their patients. Whilst this is most obvious in the use of adult kV and mAs values in CT scanning, the wide latitude now possible in exposure factors in computed and digital radiography means that less attention is also paid to optimising exposure factors for paediatric practice in plain radiography.
There are a number of published guidelines available to support general and paediatric radiologists and radiographers in this area. In the UK, national diagnostic reference levels for exposure are available for a number of common examinations ranging from chest radiographs through fluoroscopic procedures to CT, published by the Radiation Protection Division of the Health Protection Agency.
ESR: How aware are parents and relatives about the risks of radiation exposure? How do you address the issue with them?
JF: There is no doubt that parents and relatives are much better informed about the risks of radiation than they were even ten years ago, due largely to the internet and social media. Both radiographers and radiologists are regularly challenged about the risks of the examination they are planning to undertake on young patients. It is important for us to understand their concerns and to be able to explain that we use dose-minimising techniques and only expose children to radiation when we believe that the benefits of the study outweigh any potential harm. For us to be able to state this confidently, we must of course be confident in our departmental protocols, and regularly audit our practices.
It can be difficult to explain radiation risk in terms to which parents and families can relate, and it is sometimes useful to compare radiation exposure from a chest radiograph with that acquired during a trans-Atlantic flight, or background radiation. In the UK, we can also explain how living in areas such as Cornwall or the Scottish Highlands, where there are large concentrations of granite, exposes people to higher background radiation levels than living in other parts of Britain, and that undergoing a fluoroscopic examination is approximately equivalent to living in Cornwall for a year. In our department we also produce a number of leaflets that explain the examination and can help to answer parents’ concerns.
ESR: Undergoing an imaging examination, especially a long procedure like MRI, can be an uncomfortable and sometimes frightening experience for some children. How can it be made more bearable?
JF: As with any other area of the imaging department, providing a child-friendly environment in MRI is crucial in reducing children’s anxieties. This can be achieved with decorations on the wall or on the scanner itself, by having staff who know how to communicate easily with children, and by engaging the help of parents and families. Most modern scanners will allow patients to listen to their own choice of music or audio book during the procedure. This can be more practical than a parent trying to read to their child, as the noise of the scanner is better masked by headphones, but simply having a relative in the scanning room with them often provides significant reassurance.
Sometimes our referring clinicians will identify that a child is likely to be particularly frightened by an MRI, and in these cases it is very helpful to work with a play therapist to prepare the child. Letting children play with dolls and models of an MRI scanner before a visit to the MRI department is often time well spent prior to the proper scanning appointment.
ESR: How many imaging exams are performed on paediatric patients in the United Kingdom each year?
JF: A survey of imaging services for children in England, Wales and Scotland published in 2009 estimated that approximately 2 million imaging examinations are performed on children each year, of which three quarters take place in adult hospitals rather than in children’s hospitals.
ESR: Access to modern imaging equipment is important for paediatric imaging. Are hospitals in the UK equipped to provide the necessary exams?
JF: A considerable amount of investment in imaging equipment has taken place in the National Health Service over recent years, and most hospitals have access to modern equipment. Despite this, most departments struggle to keep up with evolving imaging technology, and equipment replacement programmes are often suboptimal, resulting in equipment being retained and used well beyond its ‘sell by’ date. Unfortunately, the specific needs of paediatric patients are not always recognised or considered when equipment purchasing decisions are made. Less than half of adult hospitals responding to a questionnaire in 2008 stated that they considered the requirements of children when purchasing equipment.
ESR: What has changed in paediatric radiology during your lifetime?
JF: When I was appointed 25 years ago, there were less than 30 paediatric radiologists in the UK. Now the British Society of Paediatric Radiology boasts over 200 members, both paediatric radiologists and general radiologists with an interest in paediatric imaging. Although there was a separate children’s x-ray department in my hospital, we did not even have our own ultrasound machine, and children needing ultrasound or CT examinations underwent their scans in the adult department. Of course there was no MRI available, and we were still reducing intussusceptions with barium. At that time there was a much greater dependence on fluoroscopy, and intravenous urograms and micturating cystourethrography were the mainstay of urological imaging. The introduction of MRI into paediatric imaging practice has undoubtedly revolutionised the management of paediatric patients, but in my view the greatest contribution to paediatric imaging has come from advances in ultrasound technology, which now allow us to use a non-invasive, safe, mobile procedure to image virtually every area of the body (see figures 1a & 1b).
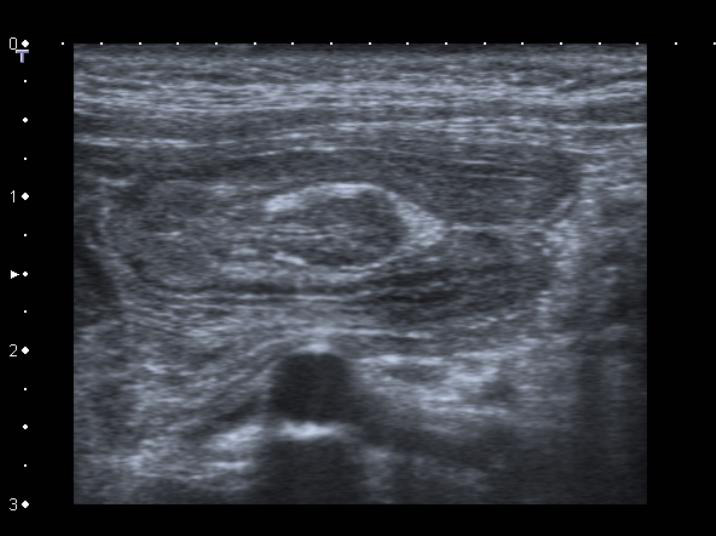
Figure 1a: High-frequency ultrasound allows us to identify pathology with exquisite detail as in this intussuscepted inverted meckel’s diverticulum.
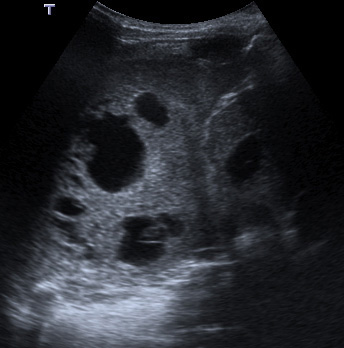
Figure 1b: Imaging of the chest no longer necessitates ionising radiation: pleuropulmonary blastoma diagnosed on ultrasound.
ESR: Where do you see the next developments in your field?
JF: In parallel with developments in adult imaging, there can be little doubt that functional imaging and quantitative image analysis in general will play a significant part in future paediatric imaging practice. In ultrasound, considerable interest is currently being shown in elastography for improved diagnosis, for example in liver and cardiac disease in childhood, and work is in progress to develop disease-specific biomarkers. In the field of suspected child abuse, finite element modelling is being explored as a means of providing objective data on many aspects of paediatric fractures. However, I believe that the greatest improvements to patient care in the imaging arena are likely to come from a more intelligent use of teleradiology, to provide specialist opinions and advice in paediatric imaging to centres without dedicated paediatric radiologists, in conjunction with the development of paediatric imaging networks between institutions. Of course none of this will be possible without a growing body of imaging professionals who are dedicated to improving imaging in children, and it will be just as important to direct our energies towards recruiting paediatric imagers, as it will be to focus on developing future technologies.
Joanna Fairhurst is a consultant paediatric radiologist at the children’s radiology department of the University Hospitals of Southampton. She undertook a fellowship in paediatric radiology at the Women & Children’s Hospital of Buffalo, New York, before taking up her consultant appointment in 1990.
Dr. Fairhurst has a special interest in dose-reduction techniques, suspected non-accidental injury, and education, and has held positions as Clinical Director of Radiology, Head of Training and Regional Educational Advisor. She is currently Chair of the Examining Board for the Royal College of Radiology, has authored and co-authored more than 60 publications and four book chapters, and is a regular reviewer for a number of radiology journals.
Read our interviews with expert paediatric radiologists from 25 different countries here


