Endovascular procedures in HCC treatment
Watch this session on ECR Live: Friday, March 8, 08:30–10:00, Room F1
There are a wide range of treatment options available when dealing with hepatocellular carcinoma (HCC), ranging from interventional and endovascular procedures to surgical interventions such as liver transplantation. The main reason for performing endovascular procedures when treating patients with hepatocellular carcinoma is the fact that liver neovascular networks are nourished exclusively by the arteries.
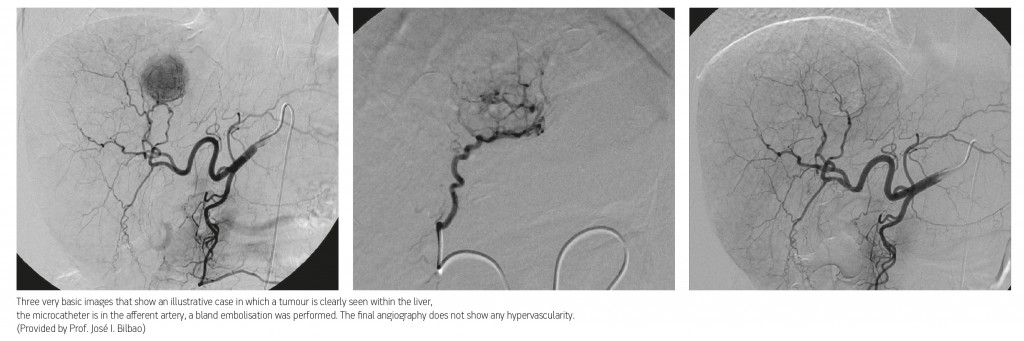
Liver tumours, both primary and metastatic, are almost entirely supplied by branches known as neo-vessels, which originate in the hepatic arteries. The surrounding peritumoural liver parenchyma is vascularised mainly by portal vein branches. When an HCC is larger than two centimetres in diameter the afferent vessel can be identified and then targeted via an arterial endovascular approach. These unique characteristics – dual vascular supply and the ability to identify the afferent vessels – are the rationale behind the use of endovascular treatments, and several different techniques have been developed over the last 30 years. Among the most frequently used are the infusion of chemotherapy and the introduction of particles, either as occluding devices or as carriers of an active agent, which attacks the tumoural cells and surrounding neovessels.
In general these procedures can be classified into three major groups: embolisation (TAE – Transarterial Embolisation), Chemoembolisation (TACE – Transarterial Chemoembolisation) and radioembolisation (TARE – Transarterial Radioembolisation).
Sometimes comparing their efficacy can be difficult, but in spite of this, a vast amount of scientific research has provided robust evidence to support the application of these endovascular techniques in patients with HCC. The best method and the appropriate subgroup of patients, remain hotly contested issues.
The interventional term embolisation refers to many different procedures. They are based on the introduction of particles that occlude the selected vessel. In liver tumours their immediate effect is ischaemia, which provokes extensive coagulative necrosis of the targeted tissue but also comes with a well-known side effect.
“The remaining, still viable, cells that survive the ischemic effect can trigger a strong pro-angiogenic mechanism through which the tumour may try to recover its pre-embolisation environment. So, the ischaemia provoked by embolisation has a proven therapeutic effect (necrosis) but also a well-known side effect, which is neo-angiogenesis, that can facilitate tumoural relapse,” said Professor José Ignacio Bilbao, ECR 2013 President, from the department of radiology at the Clínica Universitaria de Navarra in Pamplona, Spain.
Avoiding damage to the surrounding areas is of the utmost importance when ‘targeting’ the tumoural vessels. Targeting should be interpreted with two ‘optics’. There is the macroscopic method, through which all the vessels, intra and extra-hepatic, that feed the tumour are selected using a microcatheter and then the treatment is administered through them. There is also the microscopic method, in which the particle (or the active principle) is delivered as close as possible to the tumoural cells. In the case of embolisation with particles, if they are too big they may stray too far from the tumour resulting in lower necrotic/ischaemic effect and no effect on the intratumoural neovascular network.
“It is, at this moment, important to remember that in most of the HCC cases the non-tumoural liver tissue is not a healthy parenchyma and that any damage to the hepatocytes, the sinusoids or bile ducts may have severe consequences. In summary, these are the main reasons why selectivity in the treatment, widely understood, is so important in the endovascular treatment of HCC,” Prof. Bilbao pointed out.
Endovascular methods may also be used for the superselective deployment of anticancer agents for a durable occlusive effect, also known as the macroembolic effect, which is used to bring about tumoural ischaemia. There are also some other particles that are used to transport anticancer agents through the microvessels within or surrounding the tumoural nodules.
“Any transient decrease in the arterial flow, known as a microembolic effect, will not provoke any ischaemia. For example, when radioembolisation is applied, the antitumoural effect is exclusively obtained by radiation, which needs cell oxygenation (absence of ischaemia). The therapeutic effect given by the two main modalities (resin and glass), irrespective of the amount of particles deployed, is based on the delivery of Yttium-90 as close as possible to the tumoural cells,” said Prof. Bilbao.
There are new therapeutic approaches that vehiculise agents (such as pyruvate analogues) and target the metabolism of cancer cells. In theory, by using this approach the vehiculising device will not provoke any ischaemia and the agent will only be active within the tumoural cells.
Asked if there are any recent or future developments that seem promising for the treatment of hepatocellular cancer, Prof. Bilbao pointed to the use of antiangiogenic drugs. Sorafenib, and other antiangiogenic drugs, have demonstrated their efficacy, in terms of increasing responses and survival in patients with advanced HCC. There are several ongoing studies, some of which will be published soon, that have explored a possible combination of antiangiogenic drugs with endovascular treatments (chemoembolisation and radioembolisation) in non-surgical HCC cases. The reason behind this approach is that antiangiogenic drugs may decrease the neoangiogenic effect triggered by endovascular procedures. Some questions still remain unanswered; among them is whether antiangiogenic drugs should be administered before, during or after TACE and TARE.
Dr. Alberto Benito from the Clínica Universitaria de Navarra in Pamplona, who will also give a speech during the session on HCC, clarified that some uncommon radiological patterns can be seen after the use of Sorafenib, which could cause some confusion: “Sorafenib is a new drug, a multikinase inhibitor, which has improved the survival of patients with advanced stage HCC. It works as an antiproliferative and antiangiogenic drug, so one should expect a decrease in tumoural hypervascularisation with a delay in progression and an increase in survival after treatment. Although there are still no validated criteria to assess Sorafenib efficacy, functional techniques such as perfusion CT/MR or diffusion MRI, and new approaches such as the recently proposed mRECIST guidelines may be useful to evaluate patients with HCC in the near future.”
Overall the session will focus on the current management of HCC as laid out in the scientific guidelines and it will also cover the importance of a multidisciplinary approach in ensuring patients get the best treatment available. Lectures on hepatocellular carcinoma from surgical and oncologic perspectives will be given by Dr. Fernando Pardo and Prof. Bruno Sangro, both from the Clínica Universitaria de Navarra in Pamplona.
Multidisciplinary Session: Managing Patients with Cancer
Friday, March 8, 08:30–10:00, Room F1
MS 4: Hepatocellular carcinoma
• Chairman’s introduction
B. Sangro; Pamplona/ES
• Abdominal radiology
A. Benito; Pamplona/ES
• Interventional radiology
J.I. Bilbao; Pamplona/ES
• Surgery
F. Pardo; Pamplona/ES
• Hepatology/oncology
B. Sangro; Pamplona/ES
• Case presentation and discussion