B-0951 Comparison of contrast-enhanced dual-energy mammography (CEDEM) with contrast-enhanced magnetic resonance imaging (CE-MRI) in breast lesions: a prototype report
T. Knogler, R. Leithner, M. Hörnig, M. Waitzbauer, F. Semturs, G. Langs, P. Homolka, K. Pinker-Domenig, T.H. Helbich | Monday, March 11, 14:00 – 15:30 / Room F1
Purpose: To test the feasibility of CEDEM, by comparing its results with CE-MRI in breast lesions.
Methods and Materials: Fifteen female patients with 15 breast lesions were included in this study. CEDEM was performed with a Mammomat Inspiration prototype (Siemens, Germany) before and after i.v. administration of 2 ml Iomeron® 400 (Bracco, Italy) per kg b.w. at a rate of 3.5ml/sec. The same lesions were assessed with CE-MRI (Tim Trio, Siemens, Erlangen, Germany) using a standard protocol and the administration of 0.2mmol Dotarem® (Guerbet, France) per kg b.w. Images of both modalities were assessed by two readers with respect to morphology and enhancement characteristics. A histological work-up was performed in all lesions.
Results: Histopathology revealed eight malignant and seven benign lesions (size range from 8 to 38mm). Morphology and enhancement characteristics were similar and comparable with both techniques. All malignant lesions showed strong contrast uptake and suspicious morphologic signs, whereas benign lesions tend to enhance less strong on both techniques. Based on the morphologic and enhancement characteristics CEDEM and CE-MRI allowed accurate differentiation of benign and malignant breast lesions.
Conclusion: CEDEM allows adequate differentiation of benign and malignant breast lesions using morphologic and enhancement characteristics. CEDEM imaging features are comparable to those of CE-MRI. CEDEM offers a feasible and low cost alternative to CE-MRI in breast lesions.

B-0950 Clinical feasibility of contrast-enhanced dual-energy mammography (CEDEM) with a tungsten (W)/titanium (Ti) anode/filter combination: a prototype report
T. Knogler, R. Leithner, M. Hörnig, F. Semturs, M. Waitzbauer, G. Langs, P. Homolka, K. Pinker-Domenig, T.H. Helbich | Monday, March 11, 14:00 – 15:30 / Room F1
Purpose: To test the feasibility of CEDEM with a W/Ti anode/filter combination for high energy images in a clinical setting.
Methods and Materials: Fifteen female patients with 15 breast lesions were included in this study. CEDEM was performed with a Mammomat Inspiration prototype (Siemens, Germany) before and after i.v. administration of 2-ml Iomeron® 400 (Bracco, Italy) per kg b.w. at a rate of 3.5ml/sec. Dual-energy images were acquired with 28-32kVp and a W/Rhodium (Rh) anode/filter combination for low-energy and 49 kVp and a W/Ti anode filter combination for high energy. Weighted subtraction images were computed for diagnostic work-up. Images were assessed by two readers with respect to lesion-enhancement and image quality. A histological work-up was performed in all lesions.
Results: Histopathology revealed eight malignant lesions and seven benign lesions (size range from 8 to 38mm). All malignant lesions enhanced and were seen from both readers on weighted subtraction images. Benign lesions did not enhance thus they were not visualised on weighted subtraction images. Image quality was rated excellent from both readers. Based on the visibility of the lesion CEDEM allowed an accurate differentiation of benign and malignant breast lesions.
Conclusion: CEDEM with a W/Ti anode/filter combination is suitable and feasible. Lesion visibility and image quality were excellent. Further research is needed to determine the value of CEDEM in a clinical setting.

A-585 B. Peripheral skeleton
V.N. Cassar-Pullicino | Monday, March 11, 10:30 – 12:00 / Room A
In this interactive session focussing on peripheral musculoskeletal lesions presenting to the Accident and Emergency Department, we will review the strengths and weaknesses of the imaging modalities applied to chosen bone, joint and soft tissue lesions. The imaging-based approach will strengthen the understanding of the different pathological entities which vary from trauma to infection in both the paediatric and adult age groups.
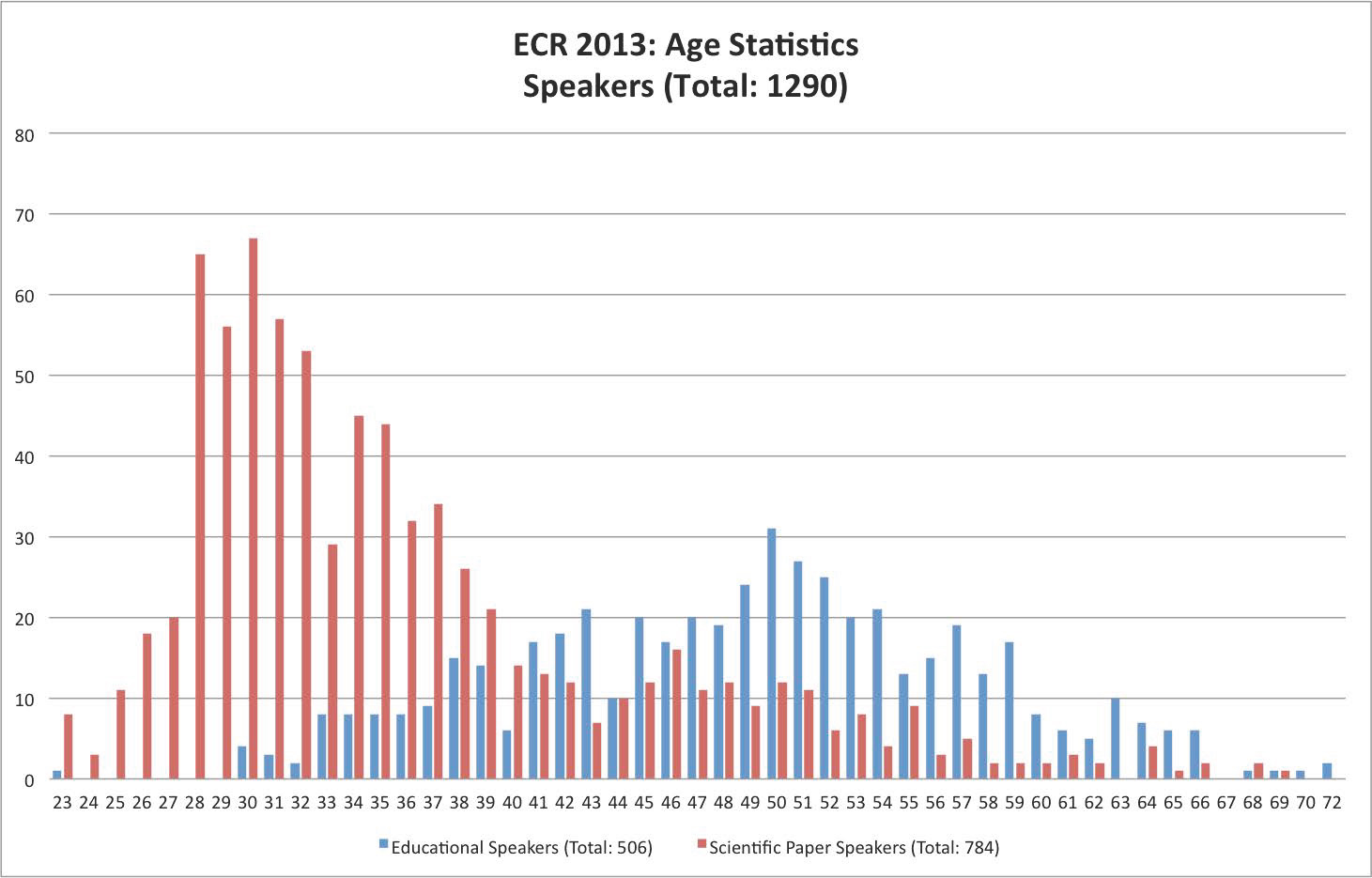
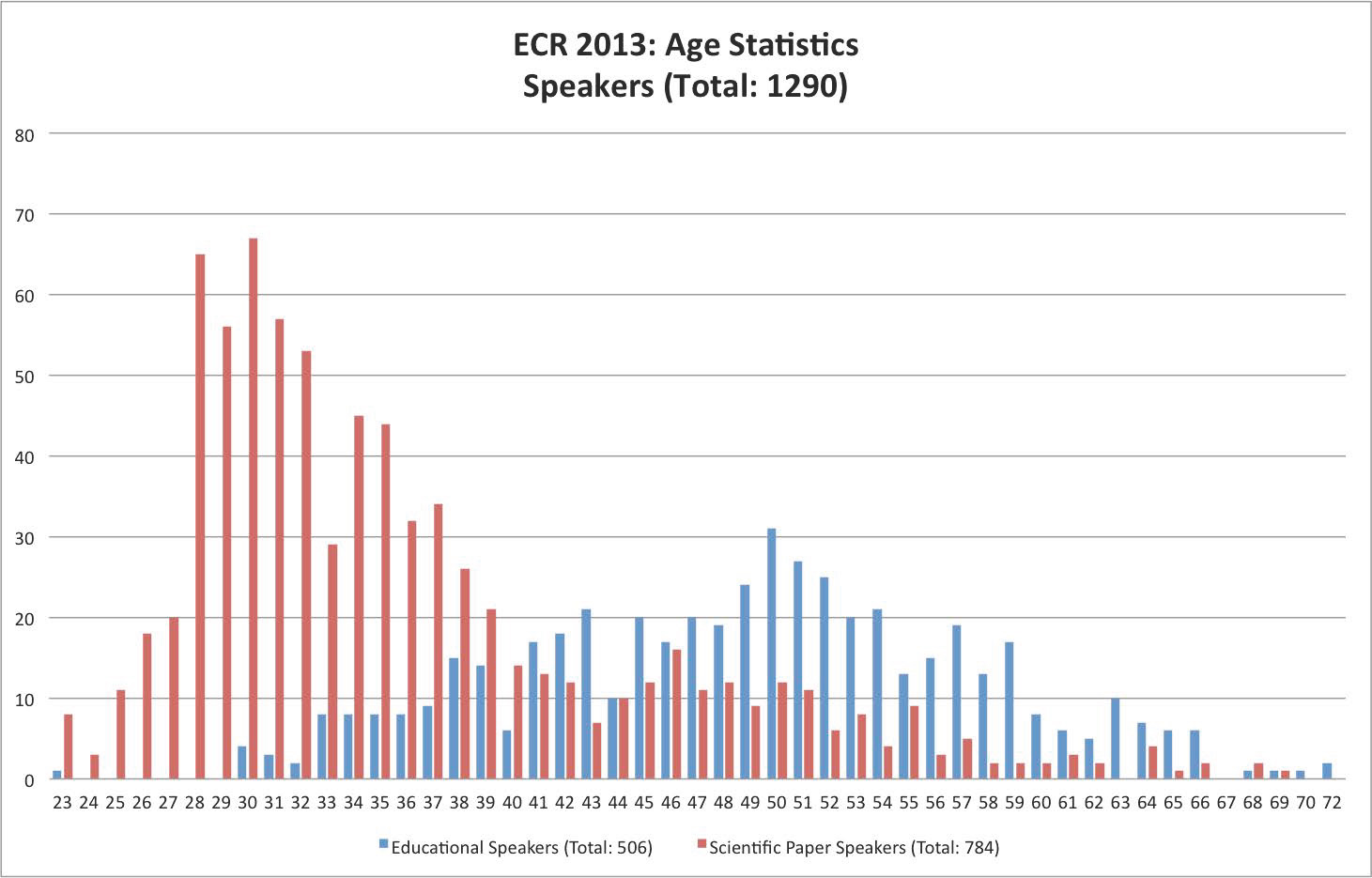
The graph below shows the ages of speakers at ECR 2013. While the most common age of scientific paper presenters was 30, the most common age among educational speakers was 50.
Your ECR future is bright: today’s presenters, tomorrow’s teachers …

The ECR represents a unique mixture of tradition, innovation and entertainment. Every year the Congress Committee and the ESR Office try to introduce some innovations to attendees. Some of these innovations are quite big and remarkable, others could be quite small and almost invisible. For example, let’s look back and recall the history of the Electronic Poster Online System (EPOS) at the ECR. In 2003, when EPOS was born and launched for the first time, there were some sceptics saying that it was a step back compared to sessions with traditional paper posters. But EPOS turned out to be extremely successful. Today we cannot imagine the ECR without EPOS. And after more than 10 years of EPOS, we consider it a unique online scientific and educational database. Seeing this success, other medical congresses have started to follow the new standard of poster presentations established by the ECR.
Read more…

A-618 C. Cystic fibrosis and other bronchiectatic diseases
M.U. Puderbach | Monday, March 11, 16:00 – 17:30 / Room I/K
Several different diseases go along with the development of bronchiectasis. Bronchiectasis may result from chronic infection, proximal airway obstruction, or congenital bronchial abnormality. In cystic fibrosis, bronchiectasis is one of the key features of lung involvement. Bronchiectasis can present with a variety of non-specific clinical symptoms, including hemoptysis, cough, and hypoxia. Bronchiectasis is defined as localized or diffuse irreversible dilatation of the cartilage-containing airways or bronchi. The imaging gold standard for bronchiectasis is thin-section CT. Morphologic criteria on thin-section CT scans include bronchial dilatation with respect to the accompanying pulmonary artery (signet ring sign), lack of tapering of bronchi, and identification of bronchi within 1 cm of the pleural surface. Bronchiectasis may be classified as cylindric, varicose, or cystic, depending on the appearance of the affected bronchi. It is often accompanied by bronchial wall thickening, mucoid impaction, and small-airways abnormalities. Besides CT, nowadays MRI of the lung is able to image the relevant morphological features of bronchiectasis. In addition, functional changes due to bronchiectasis can be studied.

Dear Friends,
Dr. Pepe refuses to leave Mexico and I have to go there to bring him back. I have asked my friends Jose Vilar and Marisa Domingo to cover for me and present this week’s case. The radiographs below belong to an 18-year-old woman with recurrent haemoptysis.
Leave your thoughts and diagnosis in the comments section and come back for the answer on Friday.
Diagnosis:
1. Arteriovenous malformation
2. Hypoplasia of left lung
3. Vasculitis
4. None of the above
Read more…
A-187 A. RF ablation
J. del Cura | Friday, March 8, 16:00 – 17:30 / Room N/O
RF ablation is currently indicated in HCC as curative treatment in Child-Pugh A-B patients with: single <2 cm nodule and not candidates for transplation, 1-3 nodules <3 cm and not candidates for resection or transplantation. RF can be also performed in patients waiting for liver transplantation. Some studies suggest that survival does not differ between RF ablation and resection in 5 cm because of the high possibility of recurrence. Different types of electrodes can be used: internally cooled, cluster, expandable, with saline instillation. Although results can be good with any of them, every type of device requires a different technique of ablation. Obtaining a margin of at least 0.5 cm of ablated tissue around the tumour is key to avoid recurrences. Combined treatments like combining chemoembolization or PEI with RFA can be useful to increase the ablation volume. Published data show a pooled 5-year survival of 48-55%, with better outcomes in Child-Pugh A patients. In candidates for surgery, 5-year survival is similar to resection: 76 %. RFA is safe: major complications appear in 10 % and reported mortality is 0.15%. Tumours located subcapsular or near major vessels, biliary tree or bowel are more prone to complications. Laparoscopic ablation can be an alternative in these cases. Imaging follow‑up with CT, MRI or CEUS is performed to assess the outcome and detect recurrences, new lesions or complications. Although not well established, most protocols include an immediate post-procedure imaging, 1-month follow-up and explorations every 3 or 6 months for 2-3 years.

A-438 A. The current criteria for nodal involvement on CT/MRI
W. Schima | Sunday, March 10, 14:00 – 15:30 / Room E2
In a variety of diseases, such as metastatic disease, lymphoma and inflammation, lymph node enlargement can be seen. Thus, lymph node characterization is important to differentiate between benign and malignant disease. It is based on size (short axis diameter) and morphologic criteria, such as shape, homogeneity, and contrast enhancement. For abdominal nodes, location-specific size criteria apply (upper limit of normal: lower paraaortic 11 mm, upper paraaortic 9 mm, gastrohepatic ligament 8 mm, portocaval space 10 mm, retrocrural space 6 mm; pelvic nodes 10 mm). However, in clinical practice, often a universal size threshold of 10 mm is used in abdominal imaging. In chest CT, an upper limit of normal of 10 mm is universally applied. However, size criteria alone are unreliable: CT for lung cancer staging has a pooled sensitvity of 51 % (i.e., false negative diagnoses of metastatic deposits in normal-sized nodes), and a specificity of 86 % (i.e., false positive diagnoses due to enlarged reactive nodes). With MRI, the same size criteria apply. However, additionally features such as central necrosis (T2w fatsat or gadolinium-enhanced images) are suggestive of metastasis (or suppurative infection). Lymph node-specific USPIO MR agents can depict tumour deposits in subcentimeter pelvic nodes. Unfortunately, they did not reach market approval. DWI is helpful in identifying in lymph nodes as they exhibit high SI with higher b-values. However, diffusion pattern of benign and malignant nodes overlap, so that ADC values do not aid in characterization. Despite the use of modern MDCT and MRI techniques, lymph node characterization needs further improvement.

Dear Colleagues, Dear Friends,
It is now just a few weeks until ECR 2014. As congress president, I am very much looking forward to welcoming you to this meeting, which will take place on March 6-10 in Vienna, Austria. Every ECR that I have attended has been a unique and unforgettable event and I am absolutely sure that ECR 2014 is going to continue this brilliant chain of outstanding meetings. I am also very proud that ECR 2014 is a jubilee meeting – it is the 20th congress in the modern history of the event, counting from the pivotal year of 1991 when it was completely re-designed and held for the first time in Vienna.
Read more…